U.S. Population Health Management Solution Market "(By Component: Software, Service; By Mode of Delivery: On-Premises, Cloud-Based; By End-Use Industry: Healthcare Provider, Payers, Employer Group; By Region: North America, Europe, Asia Pacific, Latin America, and Middle East and Africa)”- Global Industry Analysis, Size, Share, Growth, Trends, And Forecast, 2024-2032
- Category: Healthcare IT and Digital Health
- Report ID: CMR34478
- Published Date:
A prominent research firm, Cognizance Market Research, added a cutting-edge industry report on the “U.S. Population Health Management Solution Market”. The report studies the current and past growth trends and opportunities for the market to gain valuable insights during the forecast period from 2023 to 2032.
U.S. Population Health Management Solution Market Analysis:
According to cognizance market research, the U.S. Population Health Management Solution market was valued at US$ 29.70 billion in 2023 and is anticipated to reach US$ 148.23 billion by the end of 2032 with a CAGR of 19.56% from 2023 to 2032.
What is the U.S. Population Health Management Solution Market?
These healthcare IT solutions are meant to boost health results in groups of patients. Several data sources, including EHRs and claims, are brought together and checked by these tools to identify risk, guide team care through coordination and aid clinical decisions. PHM supports the change from fee-for-service to systems that pay for outcomes.
Rising numbers of chronic diseases, increasing ages among people and support from the Affordable Care Act and Medicare Shared Savings Program are driving fast growth in the U.S. market for PHM solutions. Using PHM tools, providers and payers are now committed to improving care, involving patients more, and cutting costs with early prevention and treatment.
Principal players in health information management are Optum, Oracle Health (Cerner), Epic Systems, Philips Healthcare, and Merative (formerly IBM Watson Health. These organizations compete using AI-powered cloud solutions that easily connect to the current healthcare infrastructure. Due to the fast movement toward digital healthcare, it is increasingly important for PHM solutions to boost the care patients receive and the overall health of groups.
U.S. Population Health Management Solution Market Outlook:
The growth of the U.S. Population Health Management market is being sustained by the ongoing change of the healthcare sector towards offering value-based care. Because providers are focusing more on wellness rather than illness, PHM tools are playing a key role in organizing care, lowering costs and enhancing results. Their features combine clinical, financial and behavioral information, making it easier to use data for better decisions.
Market expansion is greatly influenced by an increase in chronic disorders and an aging population. Increasingly, both healthcare providers and payers use PHM to spot individuals at high risk, design custom care plans, and handle care management more efficiently. This active form of care results in happy patients and fewer visits to the hospital or emergency room.
The PHM sector is being transformed by ongoing progress in technology. PHM tools are getting better at helping many people thanks to using the cloud, AI and telehealth. Minimal data sharing is insufficient; vendors are competing on the ability to confirm data in EHRs and other interconnected healthcare systems to ensure coordinated and joined-up care services.
Furthermore, strong measures from regulators and governments are pushing the use of crypto. Because of the Medicare Shared Savings Program and value-based payment, healthcare providers are motivated to use PHM methods. Furthermore, social determinants of health and equity are now receiving greater importance in population health planning.
It is projected that the U.S. PHM industry will grow only stronger, as more tech vendors, health systems, and insurers enter the competition. As organizations adopt digital technologies, PHM tools will enable better, more predictable, and precise patient care, becoming important factors in high-quality healthcare.
Segment Analysis:
In the U.S., the software part of the PHM solution market accounts for the biggest slice because people are now requiring better health data use, improved care coordination, and increased patient participation. The reason cloud solutions are rising in popularity is that they can be scaled, easily linked to other systems, and accessed from remote places. More and more, AI and predictive analytics are being added to these platforms to help find those at risk and choose the ideal treatment for each individual.
Among the main groups using PHM solutions, hospitals, physician groups, and ACOs lead, because they need them to manage chronic diseases, follow quality guidelines, and change to models that value quality over quantity. Payers and employer groups, too, are using health plans more to care for their members and control costs by supporting healthy actions. Since IT experts are found everywhere, there is more interest in these solutions, and more new ideas are being created.
Geographical Analysis:
Population health management (PHM) gets most easily implemented in the U.S. because the healthcare system is strong, regulations are in place, and EHRs are used everywhere. These programs from the federal government, Medicare Advantage and the Medicare Shared Savings Program, are drawing attention towards value-based care models connected to PHM adoption. Because of these factors, there are many chances for PHM solutions to continue being developed and implemented in the U.S.
California, New York, Texas and Massachusetts, due to their large regional healthcare and IT networks, are leading users of PHM platforms. They enjoy having many health organizations, research institutes and tech firms which help PHM technologies be used and improved early on. The easy access to digital tools and skilled people experienced in data-driven healthcare leads cities to adopt it more quickly.
At the same time, there are difficulties and also possibilities in rural and underserved areas of the U.S. Less effective resources and facilities in some regions may slow the adoption of renewables, but government incentives and funds are helping to fix this. More and more, PHM vendors are offering cloud-based, flexible services that make it easier to monitor patients remotely so that care reaches all parts of a region and results are improved.
The report offers the revenue of the U.S. Population Health Management Solution market for the period 2020-2032, considering 2020 to 2022 as a historical year, 2023 as the base year, and 2024 to 2032 as the forecast year. The report also provides the compound annual growth rate (CAGR) for the U.S. Population Health Management Solution market for the forecast period. The U.S. Population Health Management Solution market report provides insights and in-depth analysis into developments impacting enterprises and businesses on a regional and global level. The report covers the U.S. Population Health Management Solution market performance in terms of revenue contribution from several segments and comprises a detailed analysis of key drivers, trends, restraints, and opportunities prompting revenue growth of the U.S. Population Health Management Solution market.
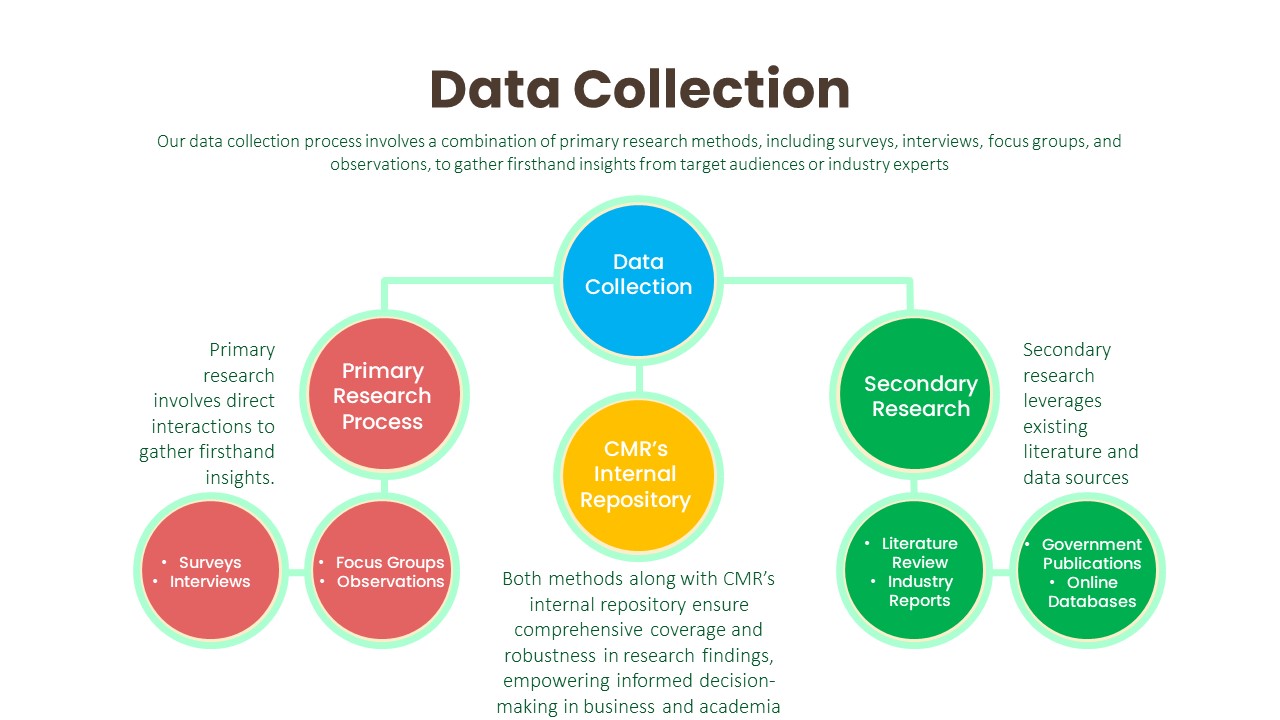
The report has been prepared after wide-ranging secondary and primary research. Secondary research included internet sources, numerical data from government organizations, trade associations, and websites. Analysts have also employed an amalgamation of bottom-up and top-down approaches to study numerous phenomena in the U.S. Population Health Management Solution market. Secondary research involved a detailed analysis of significant players’ product portfolios. Literature reviews, press releases, annual reports, white papers, and relevant documents have also been studied to understand the U.S. Population Health Management Solution Market. Primary research involved a great extent of research efforts, wherein experts carried out interviews telephonic as well as questionnaire-based, with industry experts and opinion-makers.
The report includes an executive summary, along with a growth pattern of different segments included in the scope of the study. The Y-o-Y analysis with elaborate market insights has been provided in the report to comprehend the Y-o-Y trends in the U.S. Population Health Management Solution market. Additionally, the report focuses on altering competitive dynamics in the global market. These indices serve as valuable tools for present market players as well as for companies interested in participating in the U.S. Population Health Management Solution market. The subsequent section of the U.S. Population Health Management Solution market report highlights the USPs, which include key industry events (product launch, research partnership, acquisition, etc.), technology advancements, pipeline analysis, prevalence data, and regulatory scenarios.
U.S. Population Health Management Solution Market Competitive Landscape:
There are several small and major firms participating in the highly fragmented U.S. Population Health Management Solution market. The new strategies formed by companies revolve around accuracy and precision. The following are some of the major market participants:
- Oracle Corporation
- Conifer Health Solutions
- eClinicalWorks
- McKesson
- Advisory Board
- Philips
- Athenahealth
- Welltok
- Cerner Corporation
- Epic Systems Corporation
- eClinicalWorks
The report explores the competitive scenario of the U.S. Population Health Management Solution market. Major players working in the U.S. Population Health Management Solution Market have been named and profiled for unique commercial attributes. Company overview (company description, product portfolio, geographic presence, employee strength, Key management, etc.), financials, SWOT analysis, recent developments, and key strategies are some of the features of companies profiled in the U.S. Population Health Management Solution Market report.
Segmentation:
U.S. Population Health Management Solution Market, By Component:
- Software
- Services
U.S. Population Health Management Solution Market, By Mode of Delivery:
- On-Premises
- Cloud-Based
U.S. Population Health Management Solution Market, By End-use Industry:
- Healthcare Provider
- Payers
- Employer Group
U.S. Population Health Management Solution Market, by Region:
- North America
- U.S.
- Canada
- Europe
- Germany
- U.K.
- France
- Spain
- Italy
- Rest of Europe
- Asia Pacific
- Japan
- China
- India
- Australia & New Zealand
- South Korea
- Rest of Asia Pacific
- Latin America
- Brazil
- Mexico
- Rest of Latin America
- Middle East & Africa
- GCC
- South Africa
- Rest of the Middle East & Africa
Research Methodology: Aspects
Market research is a crucial tool for organizations aiming to navigate the dynamic landscape of customer preferences, business trends, and competitive landscapes. At Cognizance Market Research, acknowledging the importance of robust research methodologies is vital to delivering actionable insights to our clientele. The significance of such methodologies lies in their capability to offer clarity in complexity, guiding strategic management with realistic evidence rather than speculation. Our clientele seek insights that excel superficial observations, reaching deep into the details of consumer behaviours, market dynamics, and evolving opportunities. These insights serve as the basis upon which businesses craft tailored approaches, optimize product offerings, and gain a competitive edge in an ever-growing marketplace.
The frequency of information updates is a cornerstone of our commitment to providing timely, relevant, and accurate insights. Cognizance Market Research adheres to a rigorous schedule of data collection, analysis, and distribution to ensure that our reports reflect the most current market realities. This proactive approach enables our clients to stay ahead of the curve, capitalize on emerging trends, and mitigate risks associated with outdated information.
Our research process is characterized by meticulous attention to detail and methodological rigor. It begins with a comprehensive understanding of client objectives, industry dynamics, and research scope. Leveraging a combination of primary and secondary research methodologies, we gather data from diverse sources including surveys, interviews, industry reports, and proprietary databases. Rigorous data analysis techniques are then employed to derive meaningful insights, identify patterns, and uncover actionable recommendations. Throughout the process, we remain vigilant in upholding the highest standards of data integrity, ensuring that our findings are robust, reliable, and actionable.
Key phases involved in in our research process are mentioned below:

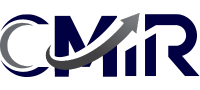
Understanding Clients’ Objectives:
Extensive Discussions and Consultations:
- We initiate in-depth discussions and consultations with our clients to gain a comprehensive understanding of their objectives. This involves actively listening to their needs, concerns, and aspirations regarding the research project.
- Through these interactions, we aim to uncover the underlying motivations driving their research requirements and the specific outcomes they hope to achieve.
Industry and Market Segment Analysis:
- We invest time and effort in comprehensively understanding our clients’ industry and market segment. This involves conducting thorough research into market trends, competitive dynamics, regulatory frameworks, and emerging opportunities or threats.
- By acquiring a deep understanding of the broader industry landscape, we can provide context-rich insights that resonate with our clients’ strategic objectives.
Target Audience Understanding:
- We analyze our clients’ target audience demographics, behaviors, preferences, and needs to align our research efforts with their consumer-centric objectives. This entails segmenting the audience based on various criteria such as age, gender, income level, geographic location, and psychographic factors.
- By understanding the nuances of the target audience, we can tailor our research methodologies to gather relevant data that illuminates consumer perceptions, attitudes, and purchase intent.
Identifying Challenges and Opportunities:
- We proactively identify the challenges and opportunities facing our clients within their respective industries. This involves conducting SWOT (Strengths, Weaknesses, Opportunities, Threats) analyses and competitive benchmarking exercises.
- By identifying potential obstacles and growth drivers, we can provide strategic recommendations that help our clients navigate complexities and capitalize on emerging opportunities effectively.
Grasping Specific Goals:
- We delve into the intricacies of our clients’ objectives to gain clarity on the specific goals they aim to accomplish through the research. This entails understanding their desired outcomes, such as market expansion, product development, or competitive analysis.
- By gaining a nuanced understanding of our clients’ goals, we can tailor our research approach to address their unique challenges and opportunities effectively.
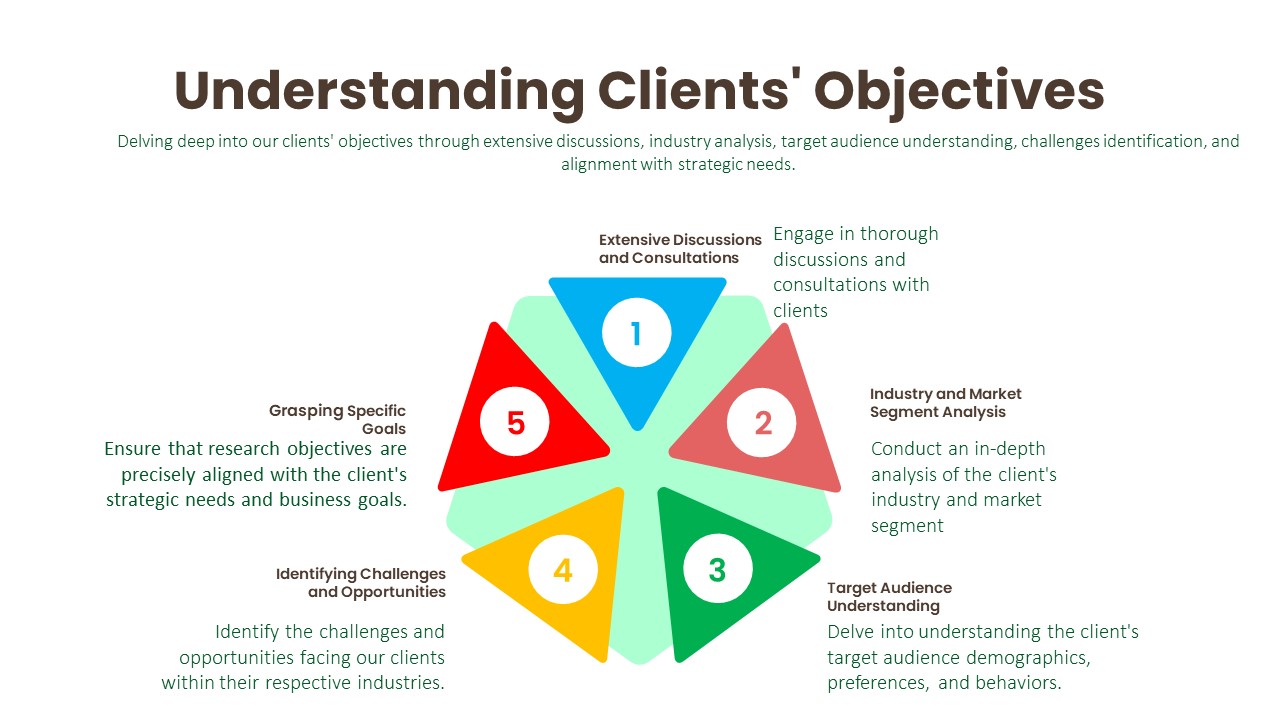
Data Collection:
Primary Research Process:
- Surveys: We design and administer surveys tailored to capture specific information relevant to our clients’ objectives. This may involve employing various survey methodologies, such as online, telephone, or face-to-face interviews, to reach target audiences effectively.
- Interviews: We conduct structured or semi-structured interviews with key stakeholders, industry experts, or target consumers to gather in-depth insights and perspectives on relevant topics. These interviews allow us to probe deeper into specific issues and uncover valuable qualitative data.
- Focus Groups: We organize focus group discussions with carefully selected participants to facilitate interactive discussions and gather collective opinions, attitudes, and preferences. This qualitative research method provides rich contextual insights into consumer behaviors and perceptions.
- Observations: We conduct observational research by directly observing consumer behaviors, interactions, and experiences in real-world settings. This method enables us to gather objective data on consumer actions and reactions without relying on self-reported information.
Secondary Research Process:
- Literature Review: We conduct comprehensive literature reviews to identify existing studies, academic articles, and industry reports relevant to the research topic. This helps us gain insights into previous research findings, theoretical frameworks, and best practices.
- Industry Reports: We analyze industry reports published by reputable trade associations (whitepapers, research studies, etc.), and government agencies (U.S. Census Bureau, Bureau of Labor Statistics, and Securities and Exchange Commission etc.) to obtain macro-level insights into market trends, competitive landscapes, and industry dynamics.
- Government Publications: We review government publications, such as economic reports, regulatory documents, and statistical databases, to gather relevant data on demographics, market size, consumer spending patterns, and regulatory frameworks.
- Online Databases: We leverage online databases, such as industry portals, and academic repositories (PubMed Central (PMC), ScienceDirect, SSRN (Social Science Research Network), Directory of Open Access Journals (DOAJ), NCBI, etc.), to access a wide range of secondary data sources, including market statistics, financial data, and industry analyses.

Data Analysis:
The data analysis phase serves as a critical juncture where raw data is transformed into actionable insights that inform strategic decision-making. Through the utilization of analytical methods such as statistical analysis and qualitative techniques like thematic coding, we uncover patterns, correlations, and trends within the data. By ensuring the integrity and validity of our findings, we strive to provide clients with accurate and reliable insights that accurately reflect the realities of the market landscape.

Transformation of Raw Data:
- Upon collecting the necessary data, we transition into the data analysis phase, where raw data is processed and transformed into actionable insights. This involves organizing, cleaning, and structuring the data to prepare it for analysis.
Utilization of Analytical Methods:
- Depending on the research objectives, we employ a diverse range of analytical methods to extract meaningful insights from the data. These methods include statistical analysis, trend analysis, regression analysis, and qualitative coding.
Statistical Analysis:
- Statistical tools are instrumental in uncovering patterns, correlations, and trends within the data. By applying statistical techniques such as descriptive statistics, hypothesis testing, and multivariate analysis, we can discern relationships and derive valuable insights.
Qualitative Analysis Techniques:
- In addition to quantitative analysis, we leverage qualitative analysis techniques to gain deeper insights from qualitative data sources such as interviews or open-ended survey responses. One such technique is thematic coding, which involves systematically categorizing and interpreting themes or patterns within qualitative data.
Integrity and Validity Maintenance:
- Throughout the analysis process, we maintain a steadfast commitment to upholding the integrity and validity of our findings. This entails rigorous adherence to established methodologies, transparency in data handling, and thorough validation of analytical outcomes.
Data Validation:
The final phase of our research methodology is data validation, which is essential for ensuring the reliability and credibility of our findings. Validation involves scrutinizing the collected data to identify any inconsistencies, errors, or biases that may have crept in during the research process. We employ various validation techniques, including cross-referencing data from multiple sources, conducting validity checks on survey instruments, and seeking feedback from independent experts or peer reviewers. Additionally, we leverage internal quality assurance protocols to verify the accuracy and integrity of our analysis. By subjecting our findings to rigorous validation procedures, we instill confidence in our clients that the insights they receive are robust, reliable, and trustworthy.
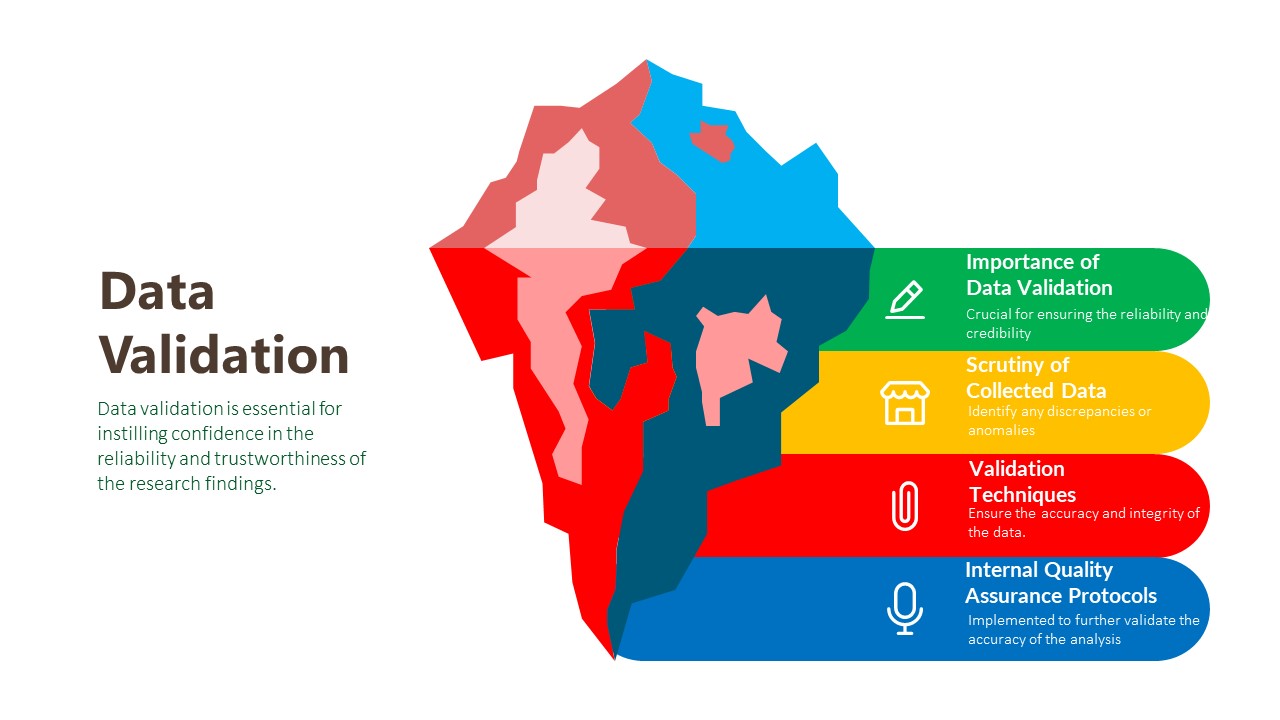
Importance of Data Validation:
- Data validation is the final phase of the research methodology, crucial for ensuring the reliability and credibility of the findings. It involves a systematic process of reviewing and verifying the collected data to detect any inconsistencies, errors, or biases.
Scrutiny of Collected Data:
- The validation process begins with a thorough scrutiny of the collected data to identify any discrepancies or anomalies. This entails comparing data points, checking for outliers, and verifying the accuracy of data entries against the original sources.
Validation Techniques:
- Various validation techniques are employed to ensure the accuracy and integrity of the data. These include cross-referencing data from multiple sources to corroborate findings, conducting validity checks on survey instruments to assess the reliability of responses, and seeking feedback from independent experts or peer reviewers to validate the interpretation of results.
Internal Quality Assurance Protocols:
- In addition to external validation measures, internal quality assurance protocols are implemented to further validate the accuracy of the analysis. This may involve conducting internal audits, peer reviews, or data validation checks to ensure that the research process adheres to established standards and guidelines.
Report Scope:
Attribute
Description
Market Size
US$ 148.23 billion (2032)
Compound Annual Growth Rate (CAGR)
19.56%
Base Year
2023
Forecast Period
2024-2032
Forecast Units
Value (US$ Million)
Report Coverage
Revenue Forecast, Competitive Landscape, Growth Factors, and Trends
Geographies Covered
North America, Europe, Asia Pacific, Latin America, Middle East & Africa
Countries Covered
U.S., Canada, Germany, U.K., France, Spain, Italy, Rest of Europe, Japan, China, India, Australia & New Zealand, South Korea, Rest of Asia Pacific, Brazil, Mexico, Rest of Latin America, GCC, South Africa, Rest of Middle East & Africa
Key Companies Profiled
Oracle Corporation, Conifer Health Solutions, eClinicalWorks, McKesson, Advisory Board, Philips, Athenahealth, Welltok, Cerner Corporation, Epic Systems Corporation, eClinicalWorks
Key Questions Answered in Population Health Management Solution Market Report
How big was the U.S. Population Health Management Solution market in 2023?
It was valued at US$ 29.70 billion in 2023.
How big will the industry size in 2032?
It is projected to reach more than US$ 148.23 billion by 2032.
What will be the CAGR during the forecast period?
It is anticipated to be 19.56% from 2024 to 2032.
What are the trends, drivers, opportunities, and challenges in the U.S. Population Health Management Solution market?
Trends: Joining AI and predictive analytics is boosting PHM by making prevention and customized treatment easier.
Driver: Because of the move to value-based care, healthcare organizations are turning to PHM tools to get better results and control their spending.
Opportunities: The growing need for interconnected, cloud platforms provides companies a way to cater to regions and places that need such services.
Challenges: Privacy challenges and system differences in healthcare prevent the smooth implementation of PHM.
What are the major players operating in the U.S. Population Health Management Solution market?
Oracle Corporation, Conifer Health Solutions, eClinicalWorks, McKesson, Advisory Board, Philips, Athenahealth, Welltok, Cerner Corporation, Epic Systems Corporation, eClinicalWorks.Global Industry Analysis, Size, Share, Growth, Trends, And Forecast, 2024-2032
We can customize every report – free of charge – including purchasing stand-alone sections or country-level reports
We help clients to procure the report or sections of the report at their budgeted price. Kindly click on the below to avail